Pain is both a sign and a stress and anxiety multiplier. In the area, the distinction in between a tranquility, lucid individual and a degrading one can be as easy as timely analgesia and skilled reassessment. The PUAEME008 Give discomfort management device sits precisely in that space. It accredits that you can evaluate, treat, monitor, and hand over a person experiencing acute pain, within the borders of your duty and neighborhood protocols. If you work in emergency situation feedback, remote medical care, sporting activity insurance coverage, event medical, or community first feedback, this brief training course can be the bridge between fundamental first aid and safe, structured pain care.
I have educated and assessed variations of this unit across ambulance accessories, industrial emergency feedback teams, and clinical assistance roles. The pupils that obtain one of the most out of it already have good scene abilities and want more confidence with analgesic representatives, paperwork, and decision-making under pressure. This breakdown goes through what PUAEME008 covers, just how it runs in technique, the common mistakes I see during analyses, and how various occupations can use it, from registered nurses and physio therapists to rescue techs and remote medics.
What the device really covers
PUAEME008 Supply pain administration is an across the country recognised unit in Australia concentrated on acute pain analysis and management in prehospital and out-of-hospital settings. It leans on three columns: systematic assessment, evidence-based intervention within scope, and continuous tracking through to handover. Unlike a broad pain management training course that dives deep right into chronic conditions, this system resolves the initial hours of care, where choices are made under time stress and with minimal resources.
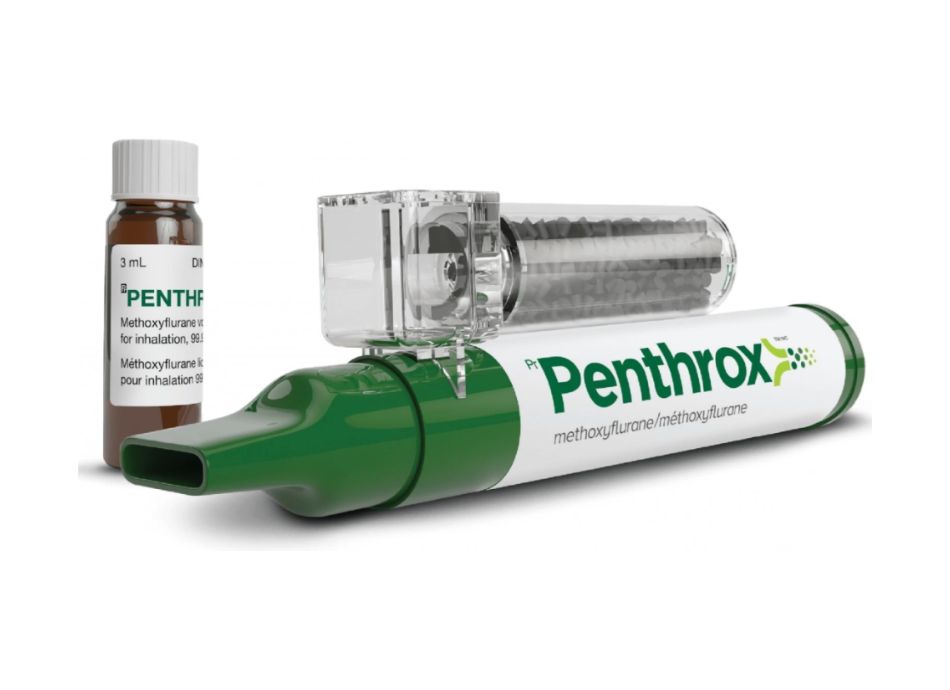
At a minimum, the performance tasks consist of examining pain using verified tools, choosing an appropriate treatment, providing analgesia or utilizing alternatives as enabled by organisational plan, keeping track of for efficiency and negative impacts, and recording and communicating the treatment and trajectory. The unit acknowledges that technique settings differ. A country first -responder might lug methoxyflurane and oral analgesics. An occasion medic might add intranasal fentanyl under a scientific governance version. The system framework pain management training for nurses permits those variants as long as the candidate shows safe, organised care.
Who advantages, realistically
You do not require a paramedic degree to obtain worth from this training course. You do need a standard of first aid or emergency care experience. People that normally sign up include students upgrading from advanced emergency treatment, mine website medics that desire structured analgesia credentials for site protocols, lifesavers and ski patrol who operate under standing orders, and allied wellness experts that work at events or remote centers and require emergency pain monitoring abilities to fill the gap between injury and definitive care.
For those scanning for details paths, the system underpins several discomfort management training programs frequently packed right into broader skill sets. It can function as a tipping stone into a certification program suffering administration for higher ranges, or as a distinct credential inside emergency situation discomfort management optional streams. For medical professionals in managed careers, it matches, instead of replaces, your professional authorisations. Registered nurses, for instance, still job under their Nurse Specialist or medical standing orders. Physiotherapists expand their emergency toolkit for sideline or remote practice however need to keep within their local policies. Treat the unit as official confirmation that you can deliver safe, fundamental to intermediate analgesia within a governance framework.
The anatomy of a brief course
Most carriers supply PUAEME008 over a small routine: pre-course reading and quizzes, eventually of in person workshops, and scenario-based assessment. Some suppliers stretch it to two days if they consist of more pharmacology and simulation. Whichever format you select, the flow is consistent. You begin with evaluation, relocate to intervention, after that to surveillance and handover. That rhythm repeats across various person presentations: isolated limb injury, abdominal discomfort, burns, back pain after hand-operated handling, and blended trauma.
Expect to exercise with pain ranges suited to different patients. Grownups with clear cognition can make use of a numerical score range, absolutely no to ten. Children or non-verbal clients may require a faces scale or observational devices like FLACC. The instructors ought to urge you secure the range with a descriptor. A 5 methods modest pain that distracts yet enables conversation; an eight is severe sufficient that the individual can not locate a comfy setting. Securing stops the common problem where every pain magically becomes a seven.

On the pharmacology side, the typical suspects appear: paracetamol, advil, methoxyflurane, and, if your supplier has the authorisation structure, intranasal fentanyl. Each representative lugs an account that you must understand well adequate to act promptly. Methoxyflurane works for brief, intense pain, has a rapid beginning, and calls for mindful mentoring on self-administration. Intranasal fentanyl offers predictable analgesia when IV accessibility is not offered, yet needs rigorous tracking for breathing depression. Oral agents take longer to work yet underpin safe, sustained relief. I have lost matter of the times early oral dosing meant that by the time we reached the ED, the patient's pain was managed without needing escalation.
Skill elements that matter on shift
Beyond analysis and memorizing recall, the program becomes muscle memory. There are five skills that I push into every friend due to the fact that they hold up in genuine cases.
- Calibrated communication: ask the appropriate inquiries at the right time, and repeat them after each intervention. "You claimed the pain was 8; after two minutes of methoxyflurane, where is it currently?" This tight loop assists capture damaging results early. Airway vigilance: also when you give agents with a broad safety margin, presume you can tip the balance. Monitor price, rhythm, effort, SpO2 if available, and responsiveness. Record the numbers, not simply your impression. Dose self-control: regard organisational protocols. If the standing order says 200 mcg intranasal fentanyl originally, confirm client age and weight cutoffs, check for contraindications, and track collective dosing versus optimums. Out in the area, distraction brings about securing mistakes; a pocket chart or mental mnemonic conserves you. Route functionality: take into consideration the atmosphere. In cold weather, intranasal absorption can be sluggish, and nasal blockage blunts impact. In great smoky settings, methoxyflurane coaching obtains shed. Pick what will certainly function here and now, not what worked last week. Handover clearness: use an organized style. I like IMIST-AMBO or an equivalent technique. State standard pain, treatment times and doses, existing discomfort rating, negative effects, and any kind of red flags you kept in mind. One min of crisp handover saves five minutes of ED investigator work.
Evidence and boundaries
A short program can not fix the whole discomfort landscape, yet it should secure you to defensible method. Proof sustains multimodal analgesia: combining acetaminophen with an NSAID offers additive benefit and decreases the requirement for opioids. In the prehospital setting, breathed in methoxyflurane and intranasal fentanyl both decrease pain rating by substantial margins within minutes. The choice rests on schedule, person factors, and provider training.
Boundaries issue. Persistent pain exacerbations are complicated. The individual might already get on opioids, and tolerance can make first-line doses really feel ineffective. The point is not to chase a no. Bring the discomfort right into a tolerable range, minimize distress, and protect against harm. For abdominal pain of unknown cause, avoid NSAIDs if there is any kind of hint of bleeding risk, anticoagulant usage, or renal concession. For head injury and modified mentation, stick to the safest agents and reduced sedation possibility, and reassess non-stop. For burns and inhalational injury risk, favor agents that permit you to keep an eye on respiratory tract without confusion, and coordinate very early transport.
Assessment mistakes I see once again and again
Cognitive overload makes wise individuals skip steps. One of the most common mistakes throughout assessment days circulation from that, not from absence of expertise. Prospects hurry into therapy without a standard discomfort rating. They choose a medicine and just after that check for contraindications. They offer methoxyflurane, then neglect hydration guidance and the maximum dosage daily. They carry out intranasal fentanyl without examining the gadget seal or priming, which causes irregular spray volume.
Another classification is documents drift. Times obtain rounded, dosages go undocumented, and the discomfort rating after therapy obtains changed by obscure language like "improved." In genuine practice, that invites risk. If the patient wears away or reports side effects, your protection is a clear record of dosages, times, impacts, and vitals over time. If you dislike paperwork, transform it into data collection. Numbers tell the tale, and they sustain clinical thinking. When puaeme008 a client's pain goes down from 8 to four after initial application and after that plateaus, you have grounds for a cautious top-up or a plan to keep with dental representatives while organizing transport.
How service providers normally structure learning
Good discomfort administration training programs keep lectures lean and push technique. Expect short modules on physiology, pharmacology, and policy, then a great deal of time on case work. You may rotate through terminals: one focused on pediatric pain analysis with developmental cues, another on intranasal distribution techniques with different atomisers, and a 3rd on scenario handover with disruptions that imitate a hectic ED. Some carriers use simulation labs with manikins and crucial indicator screens, yet a lot of will collaborate with proctors and actors. What issues is repetition till your talk track, hands, and decision-making line up without friction.

The ideal programs place you on the clock. They compress circumstances to educate quick analysis and prioritisation. That pressure, incorporated with sensible curveballs, develops behaviors you can trust. The facilitator ought to additionally debrief bluntly. If your dosage mathematics was shaky, they ought to stop the circumstance, established the estimation once again, and watch you do it without cues. Self-confidence originates from removing those wobble points now, not finding them at 3 in the early morning on a wet roadside.
Choosing a service provider that fits your world
Not all brief programs in pain management are equivalent. Seek 3 points. Initially, alignment with your local protocols and medications. There is no feeling practicing intranasal fentanyl if your solution can not authorize it. Second, trainer depth. Ask that instructs, just how commonly they practice in the area, and exactly how they manage assessment failures. Third, post-course support. A quick referral card, upgraded pharmacology sheet, and a path for refresher course training make an actual distinction six months later on when the great information fade.
If you need a discomfort monitoring certificate for employment, validate that the service provider issues a declaration of accomplishment for PUAEME008 and that your company identifies it. Some functions favor a pain administration qualification course that bundles this system with sophisticated resuscitation or oxygen therapy. If you are originating from nursing or physical rehabilitation, examine whether the company tailors case job to your settings. Sports sideline injuries require various muscular tissue memory than industrial crush injuries.
Specific notes for nurses and physiotherapists
Pain administration training courses for registered nurses and discomfort management programs for physio therapists commonly share material with PUAEME008, but your practice versions vary. Registered nurses generally run within a durable medicine governance structure. If you already offer paracetamol and ibuprofen on a ward, the uniqueness right here is not the medication, yet the setting and necessity. You will certainly practice rapid assessment, stringent monitoring after intranasal opioids, and handover from prehospital atmospheres where diagnostics are restricted. Pay additional interest to your solution's standing orders for emergency discomfort management and exactly how they fit together with the system's capability. For country and remote nurses, this device is particularly useful since it enhances your extensive technique and aids standardise assessment throughout team with wide experience ranges.
Physiotherapists in occasion or remote work face a various problem. You see severe musculoskeletal injuries greater than combined medical situations, however you still need clear analgesia pathways for cracks, dislocations, burns from tools, or back red flags. A supply discomfort monitoring program that consists of joint relocation pain strategies, splinting techniques that minimize pain without deep sedation, and safe methoxyflurane use fits well. You will also discover practical tips on patient education: how to encourage paced breathing and placing that minimizes spasm while you prepare analgesia, and how to record pain trajectories to sustain reference decisions.
When much less is more
The ideal analgesic sometimes is not a medicine. Splinting a fractured wrist properly can drop discomfort scores by fifty percent before the very first breathing. Altitude, ice bags with a barrier, and gentle immobilisation all issue. Coaching slow-moving, diaphragmatic breathing seems simplistic until you see an individual's pulse settle and their face unclench. In one mine website case, an employee with a smashed finger went from nine out of 10 pain to 5 after a proper splint and cold treatment, after that to three after methoxyflurane and paracetamol. We made use of no opioid since the trajectory informed us we were winning without it. That judgment telephone call originated from cautious review, not from a response to escalate.
Adverse effects and exactly how to stay ahead of them
Analgesics have individualities. Methoxyflurane can trigger dizziness and queasiness. Dosage within limits, ensure the individual is seated, and warn them concerning the feeling before they breathe in. Breaks in between inhalations aid control side effects while keeping effect. Intranasal fentanyl functions fast and predictably however expect breathing anxiety, especially in older clients, those with comorbidities, or anyone with concurrent CNS downers aboard. Maintain airway adjuncts, oxygen, and a strategy ready. Oral NSAIDs are reliable yet can worsen stomach problems and interact with anticoagulants. Quick evaluating questions about abscess, kidney condition, and blood thinners take much less than a min and conserve hours of trouble later.
Your tracking must mirror the threat. After intranasal opioid, check respiratory rate, SpO2, degree of consciousness, and pain rack up every couple of minutes at first, then at longer intervals if steady. After methoxyflurane, observe for postural instability and queasiness, and keep dose total amounts within daily limits based on your procedure. For oral representatives, the priority is not instant damaging results however intending the timing so you do not stack analgesics carelessly. Draw up the following 4 to six hours and communicate the plan to the client and obtaining team.
Documentation that wins respect at handover
Handover lives or passes away on framework. Practice an IMIST-AMBO design, and technique your language to be short and particular. Start with recognizing information and the device. State standard pain and the first essential set. Listing drugs with precise dosages and times. Offer the trajectory in one sentence: "Discomfort went down from eight to four within 5 minutes of inhaled methoxyflurane; no adverse effects noted; respiratory price 14 to 16 the entire time." Completed with any kind of recurring threat, like believed compartment disorder, anticoagulant use, or restricted social assistance. The emergency division does not need a novella. They need trustworthy numbers and a clean timeline.
The other half of documentation is lawful and statistical. Provider track analgesia usage, discomfort results, and negative events to fine-tune methods. Your accurate entrances help boost system performance. If your service changes from methoxyflurane to intranasal fentanyl based upon information, your notes contribute to that choice. If a regulator audits an unfavorable event, accurate documents secure both you and the service.
Refreshers and maintaining the edge
Skills decay. If you do not deliver analgesia on a regular basis, your recall of dosage varieties and contraindications blurs within months. Choose discomfort management training programs that use refresher courses, situation nights, or accessibility to on the internet microlearning. Maintain an in your area authorized quick recommendation card on your package. Update it when methods change. For personal method, construct mental representatives: on a regular strain case, run through in your head what you would certainly do if the discomfort intensified, exactly how you would certainly choose the agent, and what monitoring tempo you would certainly adopt. When a real high discomfort case appears, you will really feel as though you have already been there.
Where this fits in a broader discovering pathway
PUAEME008 is one device, not a destination. Many -responders add innovative resuscitation, oxygen treatment, and injury monitoring to stretch their ability. Some solutions package a discomfort management certification course that mixes theory, PUAEME008 Give discomfort monitoring, and organisation-specific authorisations. For those looking for a discomfort administration certification for broader technique, check whether your industry requires additional governance, like a scientific method guideline sign-off or mentorship hours. If you are constructing an individual educational program, believe in layers: fundamental first aid, discomfort monitoring, advanced life support, then unique subjects appropriate to your setting, such as burns, pediatric medicines, or remote logistics.
Real-world situation patterns you will certainly see in training
Good programs stay clear of cherry-picked easy victories. Anticipate complexity. A building and construction worker with a tibial fracture, hypotension borderline reduced from warmth, and a language obstacle. A youngster with a lower arm fracture who refuses to inhale with the mouth piece unless you turn it into a game. An older grownup with kidney impairment and severe flank pain where NSAIDs are off the table. A footballer with a disjointed shoulder that desires prompt moving on the sideline, and a coach pushing you for rate. In each, the right step looks different. Your task is to protect the client and your certificate, connect clearly, and choose the least high-risk efficient path.
One instance from a winter months event sticks out. A snowboarder provided with apparent ankle joint deformity, pain 9 of ten, and shivering that covered up an increasing respiratory system price. The group moved straight to methoxyflurane, but the mask seal was poor in the wind and the patient coughed on the first inhalation. We changed behind a windbreak, heated their hands, re-coached the breathing, and safeguarded a vacuum cleaner splint. Pain was up to five promptly. The team supplied ibuprofen and paracetamol for sustained effect, kept an eye on for dizziness, and ready transportation. No heroics, simply useful changes that matched the environment.
Cost, time, and what to expect after you pass
Prices vary by service provider and region, yet a single-unit brief program commonly rests within a small specialist growth budget. Anticipate a day out of service, maybe 2 if you pick an increased program. After successful evaluation, you must obtain a declaration of achievement. Maintain it with your credential data and upload it to any kind of employer website that tracks expertises. Some insurers and event organisers request proof of a supply discomfort monitoring program when contracting medics, so having the certification ready shortens onboarding.
More vital than the paper is the confidence you remind your team. You will discover yourself making use of less words and more structure when analyzing discomfort, reaching for the best device readily, and charting with a clarity that helps the following medical professional bring the baton. That steadiness abrades. Newer employee will duplicate your flow.
Final thoughts from the coalface
Pain is not a side quest. It shapes physiology, decision-making, and dignity. A targeted system like PUAEME008 Offer discomfort management gives you the behaviors to treat it well under incomplete problems. It premises you in safe pharmacology, hones your surveillance, and constructs a dependable handover regimen. For registered nurses, physiotherapists, first -responders, and any individual with a duty of treatment in unpredictable environments, the skills slot nicely right into daily method. Combine the system with sincere self-audit, periodic refresher courses, and an eye on your local protocols, and you will supply steadier, kinder treatment when it matters.